Dry Eye Evaluation
Where Do You Start?
To begin dry eye treatments, you and your optometrist need to know what you are up against. In our Dry Eye Evaluation, Dr. Ward will conduct a thorough examination of the eyes, looking for the signs and symptoms of dry eye syndrome. Dr. Ward will listen intently to your dry eye story, so that you can work together to find the right treatment options for you.
Evaluation includes...
- Tear Meniscus Height
- Tear Break Up Time
- Meibomian Gland Photos
- Meibomian Gland Atrophy Evaluation
- Oil Evaluation
- Demodex
- Dry Eye Treatment plan tailored to you
What is a Dry Eye Evaluation ?
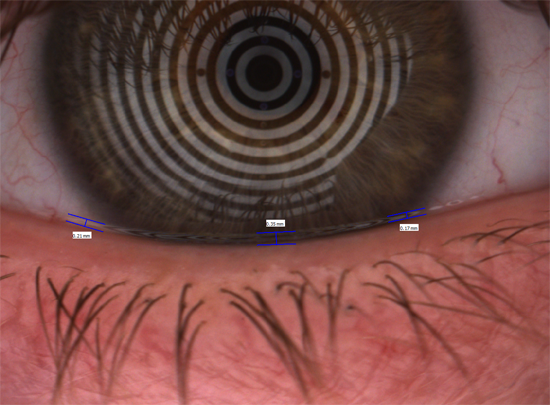
Tear Meniscus
This test allows us to evaluate the tear prism, or tear reservoir on the surface of the eye. A healthy eye has a small lake of tears, held in place by the lower eyelid. As the upper eyelid comes down, it dips into these tears, and pulls them up onto the surface of the eye. It is very common to find in dry eye that the tear meniscus is very small, and sometimes non-existent. 0.3 mm is considered normal, and anything less is a strong indicator of dry eye.
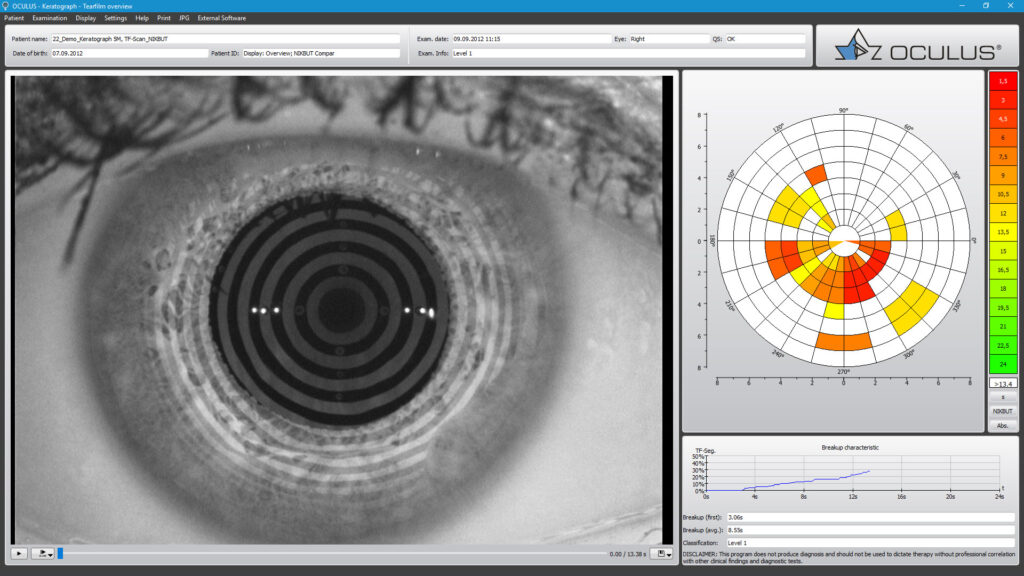
Tear Break Up Time (TBUT)
TBUT testing allows us to measure the stability of the tears on the surface of the eye. If the patient has insufficient meibum (oil) production, we will see a faster evaporation of tears.
To perform this test, we have the patient blink a couple of times, and then hold the blink for as long as they can. A healthy eye should be able to stay open for 10-15 seconds before we start to see areas of evaporation. It is not uncommon in dry eye to see the tears start to evaporate
after even only 3-4 seconds.
In the picture below, areas of red/orange indicate tears evaporating in the 3-6 second range.
Meibomian Glands Evaluation
Current research suggests that 85% of patients struggling with dry eye have a meibomian gland dysfunction. In a normal, healthy eye, the meibomian glands produce meibum, a substance similar to the color and consistency of generic vegetable oil. With each blink, a small amount of this oil is expressed from the meibomian glands and onto the ocular surface. The upper eyelid then pulls that oil over the surface of the eye. The purpose of this oil is to prevent evaporation of the tears, to create a smooth ocular surface resulting in clear consistent vision, and to decrease friction between the ocular surface and the upper eyelid.
Oil Evaluation
In Meibomian Gland Dysfunction (MGD), the oil is thick, almost like toothpaste, and can clog the glands. This results in little to no oil being expressed upon blinking. The tears on the eye evaporate quickly, causing a gritty, dry sensation, and difficulty staying comfortable in contact lenses. As part of the meibomian gland evaluation, it is necessary to evaluate the type of oil that is expressed.
Grade Scale for Meibomian Gland Dysfunction
Meibomian gland dysfunction is usually graded using the following scale. This system of grading helps the optometrist get a fuller picture of your dry eye symptoms, informing their decisions about what treatment options may be right for you.
| Grade Scale | Percentage of Blocked Glands | Quality of Meibomian Secretion |
|---|---|---|
| Grade 1 | 40%-50% | Clear to mild milky secretion |
| Grade 2 | 50%-70% | Milky to pasty secretion |
| Grade 3 | 70%-85% | Thick, pasty to very little secretion |
| Grade 4 | 85%-90% | Very little to no secretion |
Chronic blockage results in atrophy, or degeneration, of the glands. Unfortunately, gland atrophy is permanent damage. Once you lose the glands, you cannot get them back, so it’s vital to catch meibomian gland atrophy before the damage progresses too far.
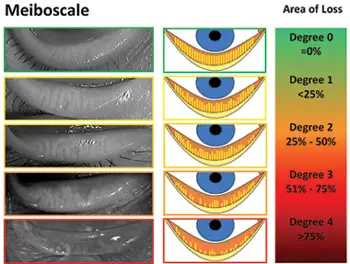
Degrees of Meibomian Gland Atrophy
The picture in the middle of the chart below is a great place to start the discussion of atrophy. The top picture (Degree 0 loss) is a healthy eye. The long yellow lines are the glands and the orange is the space between the glands. All the glands extend from the base of the lid to the lid margin. As you move down the scale (jump to Degree 4), you can see that the yellow lines are just stubs in comparison to Degree 0). Patients at grade 4 atrophy tend to be very uncomfortable, with chronic red, and irritated painful eyes. The pictures in the left hand column are the infrared photos of the real anatomy in dry eye patients. The sooner we discover the problem here, the more proactive we can be at slowing down this process.

Demodex
Demodex is a particular protozoa (think of a bug similar to bacteria) that lives on the eyelid and skin area. While bacteria on our skin is normal, this particular bug is not, and excessive amount leads to increased symptoms of dry eye. The reason is that Demodex digests skin cells, and also feeds on the meibum in the meibomian glands. What’s worse is they then procreate and lay eggs in the hair follicles of the eyelashes. This results in more demodex, and an increase in symptoms. Excessive amounts of demodex leads to:
- Color changes in the skin (Rosacea)
- Scaly Skin
- Red skin
- Sensitive or irritated skin
- Itching
- Rash
- Eye irritation
- Thickening of the eyelid
- Loss of eyelashes
This inflammation results in blepharitis. While blepharitis can manifest from a number of bacteria as well, demodex is significantly more aggressive and problematic. If you have dry eye symptoms, the likelihood of you having demodex is very high. Recent research has even noted up to 80% of individuals over the age of 60 have excessive amounts of demodex. Luckily, there are some very simply inexpensive treatments for demodex that often result in eradication of the mites if performed regularly. If you feel you might have demodex, schedule an appointment with Dr. Ward.

Schedule your Evaluation
Find Relief
Contact Us
Call us, email us, or visit our office and ask about setting up a Dry Eye Evaluation with Dr. Ward.
Get Evaluated
See Dr. Ward at our clinic where he will conduct a thorough evaluation of your dry eyes and help determine the best treatment options for YOU.
Get Treatment
Begin your treatments in whatever form they take and move one step closer to finding dry eye relief in your day-to-day life.
